Summary: ACO REACH Model Webinar
Overview and Goals
On March 22, the Center for Medicare and Medicaid Innovation (CMMI) hosted its first webinar on the Accountable Care Organization (ACO) Realizing Equity, Access, and Community Health (REACH) Model’s recently released Request for Applications (RFA). In alignment with the Biden-Harris administration, ACO REACH redesigns the Global and Professional Direct Contracting (GPDC) Model to advance health equity, health care provider leadership and beneficiary voice in model participant decisions, and robust participant screening, monitoring, and transparency. Current GPDC Model participants must have a strong compliance record and agree to meet all ACO REACH Model requirements by the performance period start date of January 1, 2023, to continue participating in the ACO REACH Model. The application period opened March 7, 2022, and will close April 22, 2022.
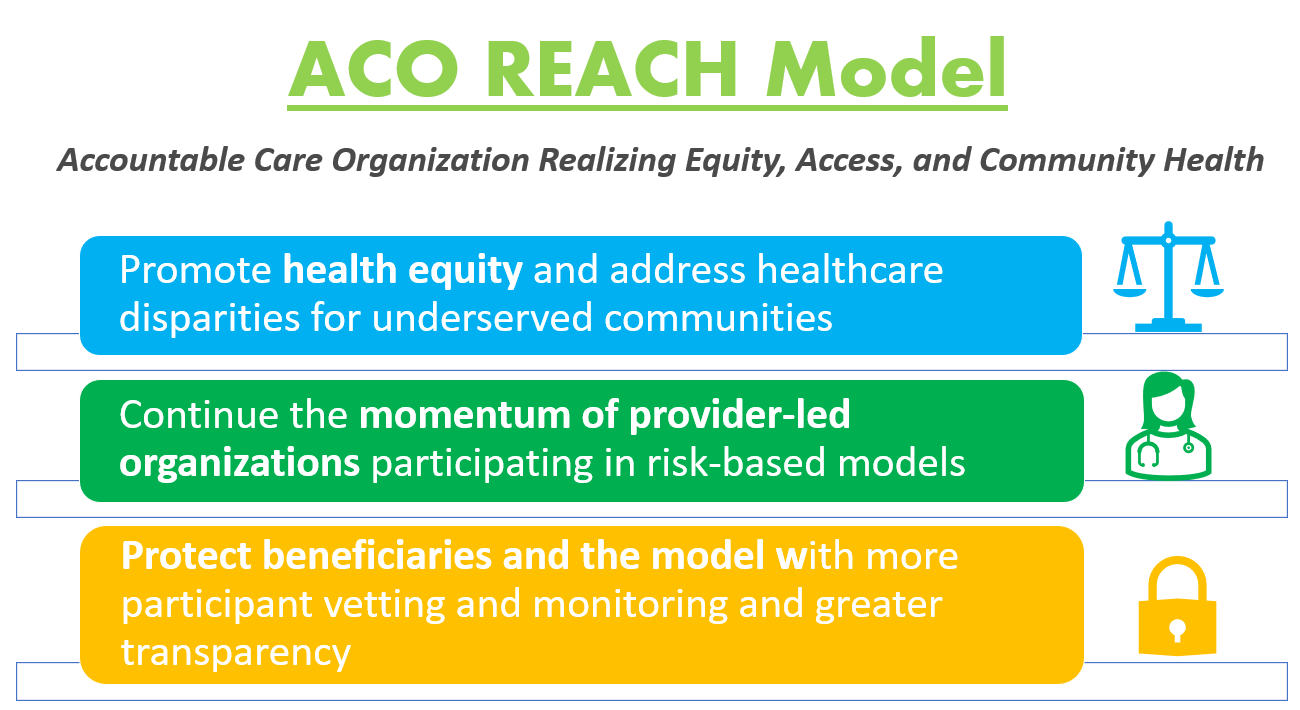
CMS’ vision for accountable care includes working with partners who share the overarching values and goal of having all Medicare beneficiaries with parts A and B in a care relationship with accountability for quality and total cost of care by 2030. The ACO REACH Model has three main goals that can inform the Medicare Shared Savings Program and future programs:
- Promote health equity and address health care disparities for underserved communities. ACO REACH will test an innovative payment approach to support delivery and coordination in underserved communities and requires all model participants develop and implement a health equity plan. The ACO REACH Model includes five health equity provisions that participants must meet: the health equity plan, health equity benchmark adjustments, health equity data collection requirements, nurse practitioner services benefit enhancements, and health equity in application scoring.
- Continue the momentum of provider-led organizations participating in risk-based models by promoting provider leadership and governance. At least 75% control of each ACO’s governing body must be held by participating providers (or their representatives), compared to 25% control that was held in the GPDC Model. Additionally, at least two beneficiary advocates must be on the governing board and hold voting rights.
- Protect beneficiaries and the model with more participant vetting and monitoring and greater transparency. There will be greater screening of applicants, monitoring of participants, and greater transparency into the model’s progress during implementation. CMS will also look into stronger protections against inappropriate coding and risk score growth.
ACO REACH Model Design Details
The redesigned model will begin its first performance year on January 1, 2023, and run for four performance years, through PY2026. A REACH ACO is defined as a legal entity identified by a tax identification number (TIN) that contracts with CMS. The ACO REACH Model offers three types of participants:
- Standard ACOs: Organizations with substantial historical experience serving Medicare beneficiaries who are aligned to an ACO through voluntary or claims-based alignment.
- New Entrant ACOs: Organizations with limited historical experience delivering care to Medicare beneficiaries and/or have not participated in fee-for-service Medicare value-based arrangements. CMS may rely primarily on voluntary alignment for this participant type.
- High Needs Population ACOs: Organizations that serve small populations of beneficiaries with complex health needs and meet additional eligibility criteria who are aligned to an ACO through voluntary or claims-based alignment.
There are two voluntary risk-sharing options in the ACO REACH Model. For each option, participating providers accept Medicare claims reductions and agree to receive some compensation from their ACO.
- Professional: lower risk-sharing arrangement, 50% savings/losses, with Primary Care Capitation Payment as the only payment option for participants. Primary Care Capitation Payment is a risk-adjusted monthly payment for primary care services provided by the ACO’s participating providers.
- Global: high risk-sharing arrangement, 100% savings/losses, with either Primary Care Capitation Payment or Total Care Capitation Payment as the payment options. Total Care Capitation Payment is a risk-adjusted monthly payment for all covered services, especially specialty care, provided by ACO’s participating providers.
CMS is committed to transparency and will be publicly sharing the following information on each ACO REACH Model: type of entity, risk-sharing arrangement, payment options, benefit enhancements, core service areas, and each organization website. CMS will share quarterly aggregated information for all REACH ACOs on quality and financial performance based on operations data and financials.
CMS is hosting more webinars in March and April to provide further in-depth information on the ACO REACH Model. All information on where and when to attend webinars, as well as the slide deck from this webinar, can be found on the CMS website.




